Future of Second Opinion in Cancer Care – Digitally coordinated patient and physician initiated model
Dr. Anjali Kulkarni, Dr. Kunal Oswal, Dr. Amol Gaikwad, Dr. Shiwani Rawat, Jyothi Borkar, et al.
Executive Summary
A patient’s experience with cancer diagnosis and care can be complicated and traumatic. It is important for a patient to remain alert and be aware about his condition, available treatment options and prognosis.
Seeking a second opinion in complex conditions will be helpful for reconfirmation and choosing the most appropriate treatment option. It enables the patients to seek evidence-based, high-quality care from a multi-specialist team of oncologists, radiologists and other competent health care professionals who can tailor cancer care for a patient’s specific needs.
As healthcare delivery shifts from a physician-centred care to a patient-centred care model , second opinion assures this transition by preventing possible errors in diagnosis and treatments that can have irreversible consequences on cancer patients.
Technology has made it possible for us to now avail a second opinion service from an oncologist sitting far away via a digital medium. Even studies suggest that the initial opinion on the diagnostics report , radiology image report and the treatment plan had changed after a second opinion was taken and the patient was able to make the right decision at the right time(1–4).
Cancer Disease Burden – A Multidimensional Problem
The term ‘Cancer’ deriving from the Greek word “Karkinos” refers to a generic Non Communicable Disease (NCD) characterised by an abnormal growth of cells in any part of the human body and in some cases gets metastasized (spread) to other parts. Being the leading cause of death globally (5), cancer exerts tremendous physical, emotional, mental and financial stress on patients, on their families, healthcare providers and on the health systems.
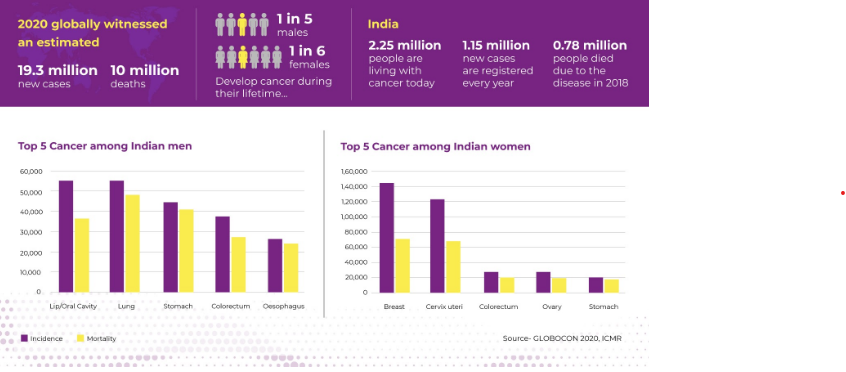
- 1 in 5 males and 1 in 6 females are developing cancer during their lifetime.
- 19.3 million new cases and 10 million deaths
- 2.25 million people are living with cancer today
- The top 5 cancers in India are
For Both Sexes – Breast cancer, Lip & Oral cavity cancer, Cervical cancer, Lung cancer, colorectal and oesophagal cancer, Stomach cancer
Male – Lip and Oral Cancer, Lung Cancer, Stomach cancer, Colorectal cancer, Esophageal cancer.
Female – Breast cancer, Cervical cancer, Ovarian cancer, Lip & Oral Cavity Cancer, Colorectal cancer, Esophageal cancer.
.
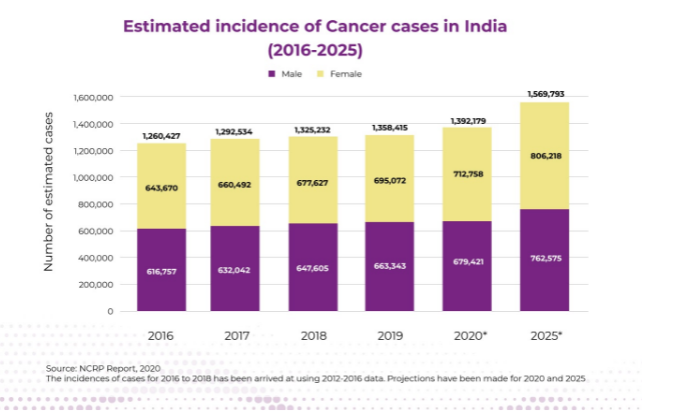
A high cancer incidence rate with a low early detection rate is a grave issue. Many health systems in the developing world are least prepared to manage this burden. While in India, the cancer burden is increasing exponentially every year, there lie many difficulties in accessing comprehensive cancer management from early diagnosis to appropriate treatment, as per the staging, for both patient and healthcare providers. Poor geographical distribution of comprehensive cancer centers is limiting the access to advanced and multimodal treatment options for patients.
A study (6) conducted on cancer statistics in India found that at the time of diagnosis majority of the patients with cancer were diagnosed as locally advanced/locoregional for breast (57.0%), cervix uteri (60.0%), head and neck (66.6%),and stomach (50.8%) cancer. Also, lung cancer was diagnosed with distant metastasis in males (44.0%) and females (47.6%). Given the fact that much of cancer survival is associated with early diagnosis, access to medical technology is a prominent policy concern for low and middle income countries (7–9).
Current Scenario
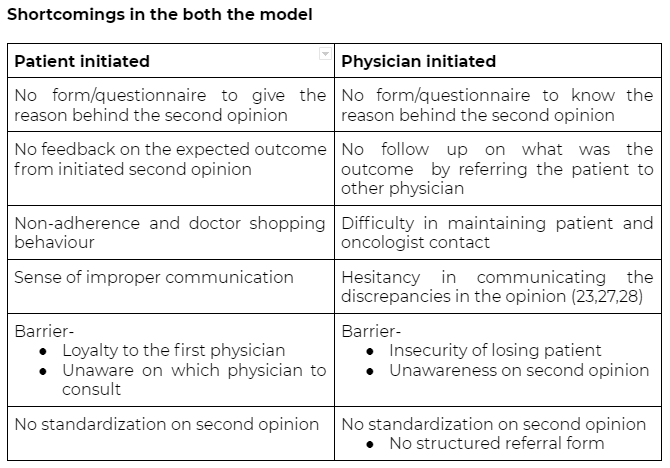
In the USA, the oncologist to patient ratio is 1:100, the UK scores 1:200, but India, on the other hand, scores 1:2000. On top of that, the majority of oncologists (cancer specialists) are available only in big cities, rendering the rural population helpless. Quality of cancer care is another critical issue that leads to poor outcomes among cancer patients. Workforce shortages in oncology, combined with an exponentially increasing number of cancer cases, reduces the sustainability of a specialist-based model of care. Delayed cancer diagnosis adds on to this burden. With no treatment in sight for advanced cancer cases, the best approach would be to ensure early diagnosis and proper treatment of patients. This would require a multidimensional approach involving the patient and his family in decision making. In this context, seeking Second Opinion is a common norm amongst the patients and their relatives to make a decision on the treatment plan. This article analyzed the variations in the need, reason, delivery models and shortcomings of two different types of Second Opinion currently practised globally.
Second Opinion for cancer care management
Advancements in cancer care are progressing at an unprecedented rate, and patients going for a second opinion on the available diagnosis before proceeding with the treatment could make a huge difference. A second opinion (also known as expert opinion) is defined as obtaining a second treatment proposal after a suggested treatment has already been presented by another physician(10) . It has become an integral part of many health-care systems and is common in cancer care. In recent years, second opinions have evolved as a patient’s right and many patients are obtaining a second opinion for a serious diagnosis. The real life study conducted on patients with Barrett’s esophagus (a high risk factor for esophageal adenocarcinoma) showed the importance of the second opinion given by the experienced pathologist in detecting Barrett’s esophagus, which is rarely diagnosed by a general pathologist(11).
Why is Second Opinion in cancer an acceptable practise?
Diagnosing cancer is complex and frightening, and so is managing it. For a patient, it then becomes important to remain informed and educated about his condition and available treatment options. With the availability of wide treatment choices and advanced procedures, cancer, today, is far more treatable than ever before.. Like advances in Genomics, Genetics, Immunotherapy, Stem Cells, and Precision Medicine.
Getting a second opinion helps to recognize available choices and make an educated decision on what is right for the patient. Given this veracity, variety and ever evolving treatment options, patients have the right to ask for a second opinion from experts. Besides therapeutic advantages, it also reassures the patient and his family and, eventually, enables them to access the most suitable treatment plan. Use of second opinion improves patient-physician relationships, enhances treatment compliance and prevents errors or negligence (8).
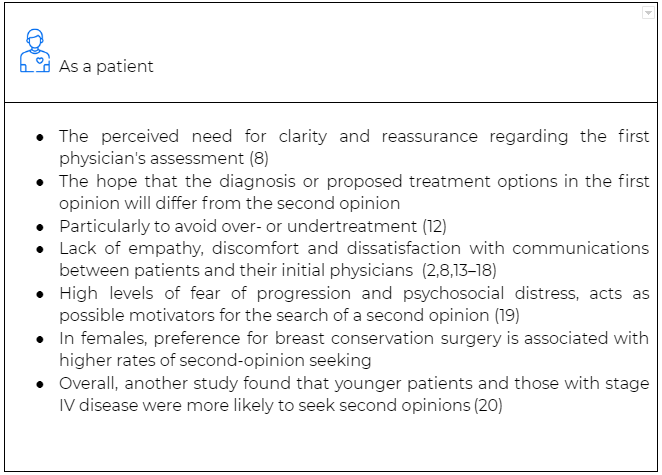
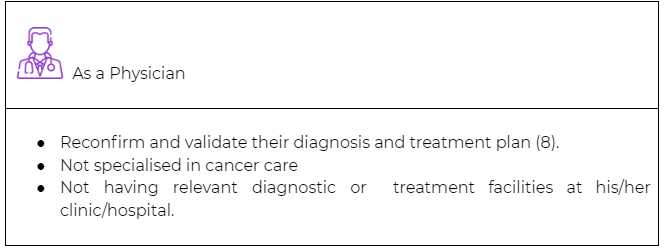
Needs, expectations for an expert opinion from a patient and a provider perspective
Expert opinion in cancer care is usually ‘ patient initiated’ or ‘physician initiated’
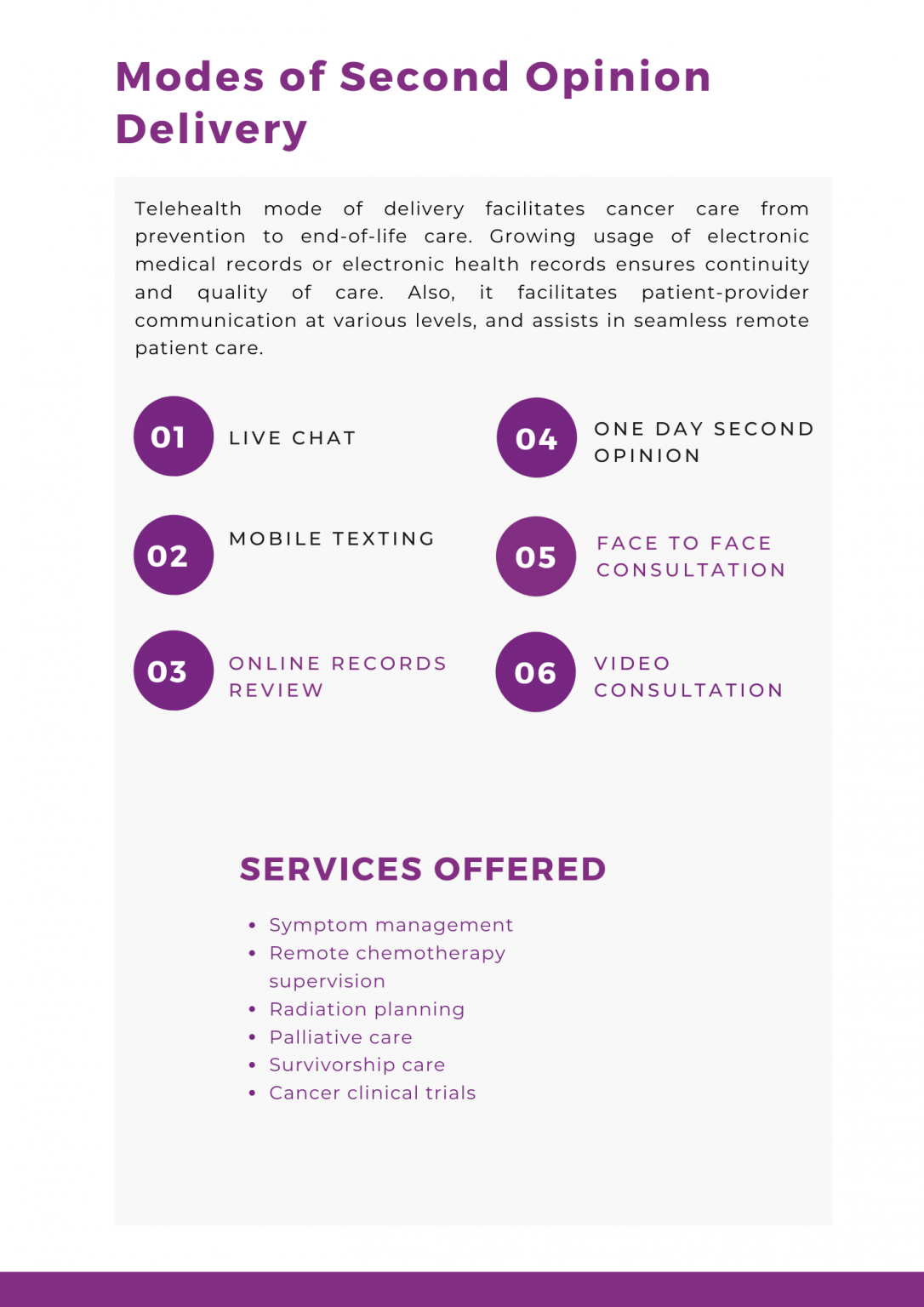
Modes of Second Opinion Delivery
Telehealth mode of delivery, facilitates cancer care from prevention to end-of-life care. Growing usage of electronic medical records or electronic health records ensures continuity and quality of care. Also, it facilitates patient-provider communication at various levels, and assists in seamless remote patient care.
- Symptom management
- Remote chemotherapy supervision
- Radiation planning
- Palliative care
- Survivorship care
- Cancer clinical trials
Barriers for the patient to seek second opinion
- Financial constraints
- State of shock
- Pressure of time to make decisions
- Trigger due to information overload resulting in apprehension of cancer patients to consult another oncologist
- Fear of jeopardizing the Patient-Physician Relationship (15,17,20,21) and obligation to the first physician are two of the most common reasons why some patients refrain from taking a second opinion
- Sometimes patients themselves tend to conceal a physician’s intentions to seek a second opinion (8,18,22)
Barriers for the physician to refer for second opinion
- Fear of losing patient (23)
- Reputation among physician network
- Lack of awareness on the second opinion, the appropriate & type of specialist to be referred (8,24–26)
- Restricted provider networks
- Preauthorization requirements
- Patient’s inability to pay
- Excessive patient travel time
- Lack of surgical subspecialists
- Not wanting to burden the patient with appointments
- Concern that referral may not be well received
- Long wait times
Legal aspect
A doctor who is asked to give a second opinion owes the patient a duty of care in the same way as the doctor who provided the first opinion. In medicolegal cases, a second opinion should be issued in accordance with the laws of the respective country. Aside from medicolegal cases, the physician should express his opinion with a clear statement that this second opinion is not for medicolegal purposes but as an approach to the question and based on the clinical judgment (29). Seeking a second opinion is the legitimate right of the patient (30,31). Patients can use the name of the first opinion and second opinion provided physician name for future litigation if any negligence (29).
A new decade, new opportunities
Arrival of a new decade presents us with an opportunity to reflect upon the progress by far in oncology and to anticipate what lies ahead. So, what are the future opportunities for global cancer control in the 2020s?
Promoting Primary Care Physician for initiating Second Opinion model
Owing to the level of expertise and experience, oncologist-led follow-up is naturally superior yet more expensive than the primary care based management (32). But people usually have a higher level of trust in Primary Care Physician (PCP) than referred physicians. Hence, the shared model of care between PCP and oncologist in treating cancer survivors (33) provides a model of cost effective care. Even studies suggest that adherence to the diagnosis or the treatment being offered depends on the effective communication and trust in the physician.
Utilizing the digital platform/communication tools are effective ways to enable communication and coordination among healthcare providers. Patients get adhered to the decisions made if PCP is involved since there is already a trust established, there will be continuity in care. Trained PCP can improve the barriers of screening , diagnosis and seeking second opinion by referring the suspected patients to the right oncologist.
- Improving access in remote areas- Primary health services covers general medicine, mild disease management, immunisation, child healthcare, and natal and postnatal care. With little to no private clinics in rural areas, a substantial portion of the rural population is virtually denied access to a doctor. In such cases, training PCP to fill gaps in healthcare delivery at the primary level is necessary. This will improve the doctor-patient ratio and provide the poorest masses in remote areas some medical assistance.
- Patient trust is high– Most of the people from both urban and rural parts of the country prefer to visit PCP to avail regular care. The trend is higher for chronic disease management and hence there is a pre-established sense of trust and belief that could be utilised.
- Screening and follow up made accessible close to home- PCPs are commonly found in private practices of rural and urban areas, thus easily accessible to all in a community. Training them to identify the risk factors, early signs and symptoms and encouraging them to conduct cancer screening camps in their area will positively be the right step in the right direction.
Another untapped resource in Indian Healthcare Scenario are the Dental & AYUSH practitioners. These practitioners can become an integral part of screening and diagnostics activities thus reducing the burden on oncologists and cancer facilities. Primary and secondary prevention, pain and palliative care, as well as supportive care during chemotherapy and radiation, are some areas where AYUSH practitioners can effectively participate.
Digital Health
Digital health systems have the ability to address existing disparities in service delivery. This new era is the ideal time for oncology focused digital technologies to address various needs of cancer patients and the community. The ideal digital health technologies will eventually aim to bridge the existing gaps in doctor- patient interaction. This reduces unnecessary clinical visits, especially to the emergency department and hospitals and promotes patient involvement in his care, generates awareness and reassures the patient and his caregivers (34).
- Teleoncology– Teleoncology has been demonstrated to improve access to care and decrease health care costs. Cancer telegenetics, remote chemotherapy supervision, symptom management, survivorship care and counselling, palliative care supervision, supervised radiation planning and approaches to increase access to cancer clinical trials are some areas suggesting successful teleoncology. It provides a platform for the rural patients to access high quality oncologist consultation from the comfort of their home thereby avoiding unnecessary travel and overhead expenses. This may also benefit a cancer patient from India to get his reports checked and verified from a specialist sitting in some other part of the world (35).
- Smart wearables- Commercially available smart wearable technologies have started to play a crucial role in helping patients manage their cancer. The American Society of Clinical Oncology (ASCO) concluded that integrating general fitness data using a Microsoft Band is a very realistic way to minimise unplanned hospitalizations in many US cancer centres. Iphones are surprisingly becoming another effective tool for oncology for(36) .
Our recommendations to enhance Second Opinion experience
- Encouraging PCP participation in cancer care management
PCP can participate in screening, diagnosing cancer and even post-cancer treatment care by periodic assessment, follow-up, remote monitoring, long term care, interpreting the laboratory test results like: blood counts, liver & kidney function etc. With the help of the digitally enabled framework PCP can seek help from radiologists, pathologists to interpret the results of the laboratory tests, and radiology images, via Teleradiology, telepathology. Also, it promotes an instant connect to the Oncologists for any cross reference and opinions in cancer care, via virtual consultation. Digital platforms enable the PCP to repeat prescriptions for those patients who stay in remote/inaccessible areas. Skilled & trained PCP can be a powerful partner in handling mental wellbeing of cancer patients and their caregivers by providing counselling and lifestyle modifications. Training on cancer risk assessment, yearly detection and appropriate management/referral and palliative care to the primary care physician may increase the physician initiated second opinions. So incorporating the PCP in cancer care would really help by directing the patients to the right oncologists. - Network coordinated model will enhance Patient initiated SO
The “Second Opinion Medical Network” is an effective decision-support method, not only to accomplish re-evaluation of the patient’s condition and subsequent enhancement of medication and prognosis, but also to prevent needless surgery and costs. Coordination of care requires being able to take information from a variety of sources. As studies say lack of communication is the main reason for doctor shopping behaviour of the patient, there is a need for clear communication between the patient and physician . Physicians must explain the diagnosis and treatment options thoroughly to the patient. For every diagnostic report oral explanations must be followed by the written report. It creates trust and promotes an interactive doctor patient relationship.
Coordinated care may include-
- 24/7 access to clinical staff to see the medical record, and answer questions about treatment, including cancer treatment side effects and other issues.
- Patient navigators to coordinate care within and outside the oncology clinic with primary care physicians & other clinical teams for any other chronic or acute health conditions that the patient has.
- Incorporating multidisciplinary tumor boards with care coordinators will improve the efficiency of the process and ensure optimization of the cancer care.
- A standardised treatment protocol among the coordinated cancer network may reduce the errors and improve efficiency
- A platform that provides the service of a second opinion, and regular follow up for the patient even after the services rendered for the outcome like an example National registry or database to enter/register the patient initiated and physician initiated second opinion request.
In Conclusion
Second opinion in a complex disease like Cancer is here to stay! Ultimately, the goal for a patient and his family is not just to survive but to thrive. There are a number of moving parts in the gamut of cancer management and to improve evidence based care a well-coordinated and highly informed system is crucial. Hence understanding the merits and demerits of Physician-led and Patient-led Second Opinion seeking behaviour, there is a huge need to assist these models to make it a mainstream care process for Oncology. Physician-led Second Opinion is very important for democratizing cancer care while it presents an opportunity for better adoption to evidence-based care and skill improvement. Patient-led Second Opinion in an assisted environment helps realize the value for money, improved communication and make the care more patient-centric.
